Premier Healthcare Specialists- Healing is Our Specialty
Advanced wound care services represent the pinnacle of comprehensive and specialized wound management. Our services are designed to address complex wounds that require specialized attention and the latest advancements in medical science and technology. Advanced wound care involves a multidisciplinary approach, often with a team of wound care specialists, nurses, and healthcare professionals who collaborate to create tailored treatment plans. These services encompass a wide range of cutting-edge therapies and treatments, including negative pressure wound therapy, hyperbaric oxygen therapy, bioengineered skin substitutes, and growth factors, among others.
Advanced wound care is distinguished by its emphasis on optimizing the wound healing process, preventing complications, and improving patients' quality of life. It provides hope and effective solutions for individuals with challenging wounds, offering the best available treatments to promote complete and rapid healing.

Types of Wounds Treated
- Arterial wounds (caused by narrowed arteries that decrease blood flow to the wound)
- Venous wounds (caused by abnormal veins leading to inflammation and swelling)
- Diabetic lower extremity wounds (caused by decreased sensation leading to repeated injury)
- Diabetic ulcers
- Surgical dehiscence or non-healing wounds
- Traumatic wounds (related to injuries)
- Complex skin tears
- Cellulitis/dermatitis
- Pressure wounds (caused by unrelieved pressure over bony prominences)
- Minor burns
- Atypical wounds (like vasculitis, pyoderma gangrenosum, and Warfarin necrosis)
- Radiation wounds
- Peristomal skin ulcers
- Non-healing wounds on any body part

Treatments and Therapies
- Total contact casting for some diabetic foot ulcers
- Negative pressure wound therapy (Wound VAC)
- Compression therapy
- Wound care and debridement
- Application of skin substitutes/grafts
- Non-invasive vascular assessment
- Bone, skin, and wound infection
- Specialty dressings
- Wound cultures and biopsies
Additional Services
- Diabetes counseling
- Skin Care
- Diabetic foot evaluation
- Nutrition education
- Smoking cessation
- Basic wound care
- Preventative foot care-nail trimming, callous removal
- Ostomy education and management
- In-service training & Educational Seminars

Arterial Wounds:
An arterial wound, also known as an ischemic wound or arterial ulcer, is a type of chronic wound that results from insufficient blood flow to a specific area of the body, typically caused by arterial disease or atherosclerosis. Arteries carry oxygen-rich blood from the heart to various parts of the body, and when there is a blockage or constriction in these arteries, the affected tissue receives inadequate oxygen and nutrients, leading to tissue damage and the development of arterial wounds. Here are some key characteristics of arterial wounds:
1. Location: Arterial wounds often occur in areas farthest from the heart, such as the lower extremities, feet, and toes, where blood flow is reduced due to the distance it must travel.
2. Appearance: Arterial wounds usually present as deep, punched-out ulcers with well-defined, regular borders. They may appear pale or yellowish due to reduced blood supply, and the surrounding skin can be cool to the touch.
3. Pain: Patients with arterial wounds often experience severe pain, especially when at rest or during periods of decreased blood flow, such as when the legs are elevated.
4. Tissue Necrosis: Arterial ulcers are characterized by tissue necrosis, with the wound bed often containing non-viable tissue. Gangrene, a condition where tissue dies due to lack of blood flow, may be present in severe cases.
5. Slow Healing: These wounds tend to heal very slowly, if at all, due to the ongoing insufficient blood supply.
6. Risk Factors: Arterial wounds are commonly associated with risk factors such as smoking, diabetes, hypertension, high cholesterol, and a history of cardiovascular disease.
7. Clinical Assessment: A healthcare provider will assess the wound's blood supply and may use diagnostic tests like ankle-brachial index (ABI) or Doppler ultrasound to measure blood flow and assess the severity of arterial disease.

Management of arterial wounds involves addressing the underlying arterial disease to improve blood flow. This may include lifestyle modifications, medications to manage risk factors, and, in severe cases, interventions like angioplasty or bypass surgery to restore blood flow. Wound care for arterial ulcers focuses on debridement (removal of dead tissue), managing infection, and promoting tissue regeneration.
It's essential for individuals with arterial wounds to seek medical attention promptly, as these wounds can lead to severe complications if left untreated. A multidisciplinary approach involving vascular specialists, wound care experts, and other healthcare professionals is often necessary to effectively manage arterial wounds and promote healing.
Venous Wound:
A venous wound, also known as a venous ulcer or stasis ulcer, is a type of chronic wound that results from venous insufficiency or dysfunction in the veins of the lower extremities. Venous insufficiency occurs when the valves in the leg veins do not work properly, leading to poor blood circulation and an accumulation of blood and fluid in the lower legs. Over time, this condition can result in venous wounds. Here are some key characteristics of venous wounds:
1. Location: Venous wounds are typically found in the lower legs, particularly around the ankles and on the inner side of the calf. These areas are most affected by venous insufficiency.
2. Appearance: Venous ulcers often appear shallow and irregular in shape, with uneven, sloping borders. The wound bed may be red or pink, and there may be hemosiderin staining, which presents as brownish discoloration of the skin.
3. Exudate: These wounds can produce moderate to high levels of exudate, which may be clear or serous, but can also become thick, yellow, or green if infected.
4. Pain: Patients with venous ulcers may experience pain, typically described as aching or throbbing. Pain is often relieved when the legs are elevated.
5. Edema: Edema, or swelling of the lower legs, is a common symptom of venous insufficiency and may be present in individuals with venous wounds.
6. Risk Factors: Risk factors for venous wounds include a history of deep vein thrombosis (DVT), obesity, family history of venous insufficiency, and occupations requiring prolonged periods of standing or sitting.
7. Clinical Assessment: Healthcare providers may use techniques like duplex ultrasound to assess blood flow in the legs and confirm the presence of venous insufficiency.

Management of venous wounds primarily focuses on improving venous circulation and promoting wound healing. This may involve the following:
Compression therapy: Applying compression bandages or stockings to reduce edema and improve venous blood flow.
Wound care: Cleaning and dressing the wound appropriately, with a focus on maintaining a moist wound environment.
Elevation: Keeping the legs elevated when sitting or lying down to reduce swelling and pain.
Lifestyle modifications: Encouraging regular exercise, weight management, and smoking cessation to improve overall vascular health.
Venous ulcers can take time to heal, and it is essential for individuals with these wounds to seek medical attention and follow a care plan provided by healthcare professionals. A multidisciplinary approach, including vascular specialist is often necessary to effectively manage Venous wounds and minimize complications.
Diabetic Wound
A diabetic foot ulcer is a common and serious complication of diabetes characterized by open sores or wounds on the feet. It typically occurs in individuals with diabetes when prolonged high blood sugar levels lead to nerve damage (neuropathy) and poor blood circulation (peripheral arterial disease). These factors can make the feet vulnerable to injuries and slow the healing process, resulting in diabetic foot ulcers. Here are some key characteristics of diabetic foot ulcers:
1. Location: Diabetic foot ulcers are most commonly found on the soles of the feet, particularly under pressure points like the heels and balls of the feet. They can also develop on the tops and sides of the feet or between the toes.
2. Appearance: Diabetic foot ulcers vary in size and depth. They may appear as shallow sores or deep craters with irregular borders. The wound bed can be pink, red, or yellowish, and the surrounding skin may be callused or discolored.
3. Exudate: These wounds can produce varying amounts of exudate, which may be clear, serous, or purulent if infected.
4. Pain or Numbness: Diabetic foot ulcers can be painful, but they can also be painless due to neuropathy. This lack of pain sensation can lead to delayed wound detection.
5. Risk Factors: Risk factors for diabetic foot ulcers include uncontrolled diabetes, neuropathy, poor circulation, smoking, obesity, and a history of foot deformities or previous ulcers.
6. Infection: Diabetic foot ulcers are prone to infection, which can lead to cellulitis or more severe complications like osteomyelitis (bone infection).
7. Clinical Assessment: Healthcare providers often use various diagnostic tests, such as the monofilament test to assess sensation, and Doppler ultrasound to evaluate blood flow, to determine the severity of neuropathy and vascular issues.

Management of diabetic foot ulcers involves a multifaceted approach to promote wound healing, prevent infection, and prevent recurrence. It typically includes the following:
Wound care: Cleaning, debriding, and dressing the wound appropriately.
Infection control: Administering antibiotics if an infection is present.
Pressure offloading: Using specialized footwear or orthotics to reduce pressure on the ulcer.
Blood sugar control: Achieving and maintaining target blood glucose levels to support healing.
Vascular interventions: In some cases, revascularization procedures may be necessary to improve blood flow.
Diabetic foot ulcers can be challenging to manage and may require ongoing care and vigilance to prevent complications. Regular foot inspections, proper footwear, and patient education on foot care are essential components of preventing these ulcers and reducing the risk of amputation. Individuals with diabetes should consult with healthcare professionals for comprehensive care and management of diabetic foot ulcers.
Surgical Dehiscence
Surgical dehiscence, also known as wound dehiscence, is a medical term that refers to the spontaneous opening or separation of a surgical incision or wound that was previously closed. This condition typically occurs within the first few days or weeks following surgery and poses a significant risk to the patient. Surgical dehiscence can vary in severity, from a small separation of the wound edges to a complete rupture of the incision. Here are some key characteristics and considerations related to surgical dehiscence:
1. Causes: Several factors can contribute !o surgical dehiscence, including:
- Tension on the wound due to inadequate closure.
- Infection or wound contamination.
- Poor tissue perfusion (inadequate blood supply).
- Underlying medical conditions, such as obesity, diabetes, or malnutrition.
- Excessive physical strain or strain on the incision site.
2. Signs and Symptoms: The signs of surgical dehiscence may include:
- Separation or gaping of the wound edges.
- Exposure of underlying tissues, organs, or surgical sutures.
- Increased pain or discomfort at the incision site.
- Drainage or oozing from the wound.
- Signs of infection, such as redness, warmth, swelling, or the presence of pus.
- A palpable "step-off" or a feeling of a gap at the incision site.
3. Complications: Surgical dehiscence can lead to various complications, including:
- Increased risk of wound infection, which can progress to more severe complications like abscesses or cellulitis.
- Delayed healing and prolonged recovery.
- Increased risk of hernia formation at the incision site.
- Exposure of internal organs, leading to potential injuries or complications.
4. Management: The management of surgical dehiscence may involve:
- Re-closure of the wound if feasible and appropriate, possibly with the use of sutures, staples, or other closure methods.
- Treatment of any underlying infection or inflammation.
- Addressing contributing factors, such as optimizing the patient's nutrition or managing chronic conditions.
- Close monitoring for signs of infection or other complications.
- In severe cases, surgical intervention may be required to address exposed organs or tissues.
5. Prevention: Preventing surgical dehiscence is essential and can be achieved through meticulous surgical techniques, proper closure methods, infection control, and careful postoperative wound care. Patients are often advised to avoid activities that place excessive strain on the incision site during the initial healing period.
Surgical dehiscence is a serious surgical complication that requires immediate medical attention. Patients who experience signs of wound separation or other related symptoms should contact their healthcare provider or surgeon promptly to evaluate and address the issue to minimize the risk of further complications and promote proper wound healing.
Pressure Wounds:
Pressure wounds, also known as pressure ulcers, decubitus ulcers, or bedsores, are localized areas of damage to the skin and underlying tissue caused by prolonged pressure and friction on the affected area. These wounds typically develop over bony prominences where the skin and tissue are compressed between the bone and a surface, such as a bed or chair. Pressure wounds often affect individuals who have limited mobility, are bedridden, or use a wheelchair. Here are some key characteristics and considerations related to pressure wounds:
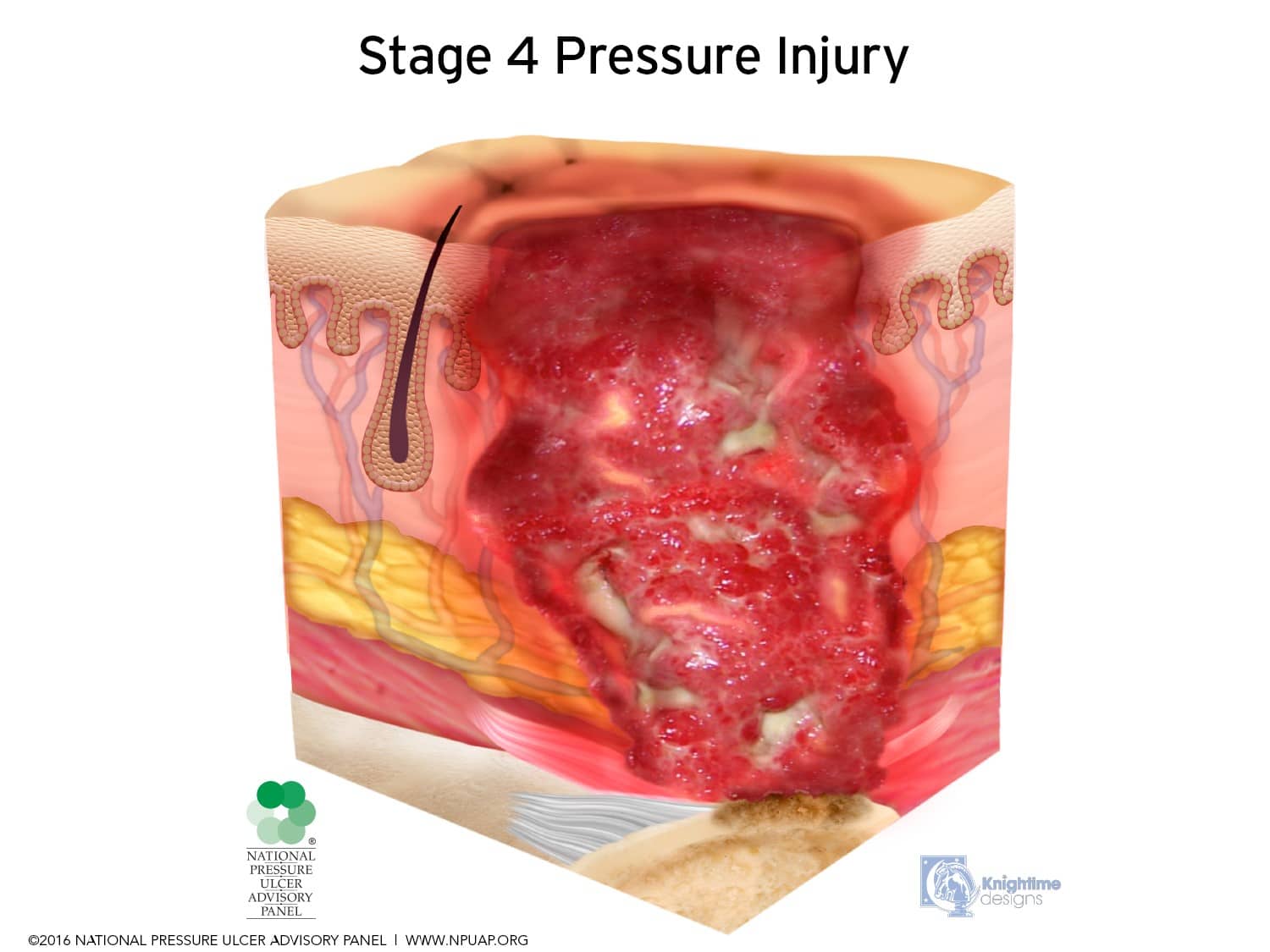
1. Stages: Pressure wounds are classified into stages based on their severity, as defined by organizations like the National Pressure Ulcer Advisory Panel (NPUAP). These stages range from Stage I (the mildest) to Stage IV (the most severe), with unstageable and suspected deep tissue injury stages also recognized.
2. Risk Factors: Factors that increase the risk of developing pressure wounds include immobility, advanced age, malnutrition, incontinence, poor blood circulation, and certain medical conditions such as diabetes and paralysis.
3. Location: Pressure wounds often develop over areas where bones are close to the skin's surface, such as the sacrum (tailbone), heels, elbows, hips, and the back of the head. The location of the wound can vary depending on a person's positioning and mobility.
4. Appearance: The appearance of a pressure wound can vary based on its stage and severity. Common characteristics include redness or discoloration (Stage I), shallow or deep open sores (Stage II-IV), tissue damage extending into muscle or bone (Stage Ill-IV), and sometimes eschar or slough, which are dead tissue coverings that can obscure the wound's depth (unstageable).
5. Pain: Pain is not always a reliable indicator of pressure wounds, especially in the early stages, as individuals with reduced sensation or neuropathy may not feel pain. However, pain can be a symptom in some cases, particularly when the wound becomes infected.
6. Complications: Pressure wounds can lead to various complications, including cellulitis (skin infection), osteomyelitis (bone infection), sepsis, and delayed wound healing. These complications can be life-threatening.
7. Prevention: Prevention is a crucial aspect of managing pressure wounds. Strategies include regular repositioning of individuals to relieve pressure, maintaining proper skin hygiene, using pressure-relieving support surfaces (such as specialized mattresses or cushions), optimizing nutrition, and providing appropriate care for incontinence.
8. Treatment: The management of pressure wounds involves wound care, which includes cleaning, debridement (removing dead tissue), applying dressings, and managing infection. In severe cases, surgical intervention may be required to promote healing and address deep tissue involvement.
Pressure wounds are a significant healthcare concern, and healthcare providers, caregivers, and individuals at risk should be vigilant in their efforts to prevent, assess, and manage these wounds. Early intervention and a multidisciplinary approach are critical in addressing pressure wounds and minimizing their impact on overall health and well-being.
Peristomal:
Peristomal skin breakdown, also known as peristomal dermatitis or stomal dermatitis, is a skin condition that occurs around an ostomy site. An ostomy is a surgical procedure in which an artificial opening (stoma) is created in the abdomen to divert the flow of waste (such as feces or urine) from the body when the normal route, such as the rectum or bladder, is dysfunctional. Peristomal skin breakdown can develop due to a variety of factors, including irritation, friction, or exposure to bodily waste. Here are some key characteristics and considerations related to peristomal kin breakdown:
1. Location: Peristomal skin breakdown occurs in the area immediately surrounding the stoma, where the ostomy appliance, such as a colostomy or urostomy pouch, is attached to the skin.
2. Causes: Several factors can contribute to peristomal skin breakdown, including:
- Irritation: Prolonged exposure to bodily waste or leakage from the ostomy appliance can irritate the skin.
- Friction: The adhesive or wafer used to secure the ostomy pouch can rub against the skin and cause irritation.
- Allergic reactions: Some individuals may be sensitive or allergic to the adhesives, pouch materials, or ostomy accessories used.
- Skin moisture: Excess moisture from perspiration or urine can soften the skin and make it more prone to damage.
3. Appearance: Peristomal skin breakdown can present as redness, irritation, maceration (softening of the skin), and, in more severe cases, erosion, ulcers, or open sores around the stoma. The skin may be painful, itchy, or have a burning sensation.
4. Risk Factors: Factors that increase the risk of peristomal skin breakdown include improper ostomy pouch fit, use of incompatible or irritating products, skin sensitivity, and a lack of proper stoma care and maintenance.
5. Management and Prevention: Managing and preventing peristomal skin breakdown involve several strategies, including:
- Ensuring a proper fit and seal of the ostomy pouch.
- Using ostomy products designed for sensitive skin if needed.
- Maintaining good hygiene, including proper stoma cleaning and drying.
- Using barrier creams or protective films to create a protective layer between the skin and the pouch.
- Addressing allergies or sensitivities to ostomy products.
- Seeking guidance from a healthcare provider or ostomy nurse to address specific issues.
Proper stoma care and the use of appropriate ostomy supplies are essential in preventing and managing peristomal skin breakdown. Individuals with an ostomy should work closely with healthcare professionals, such as an ostomy nurse, to receive education and support in ostomy care and skin protection. Early intervention and the selection of suitable ostomy products can help maintain healthy peristomal skin and improve overall quality of life for ostomy patients.
Cellulitis/Dermatitis:
Cellulitis is a common and potentially serious bacterial skin infection that affects the deeper layers of the skin and the subcutaneous tissues. It typically occurs when bacteria, most commonly Streptococcus or Staphylococcus species, enter the skin through a break or opening, such as a cut, insect bite, or scratch. Cellulitis is characterized by the following features:
1. Symptoms: Common symptoms of cellulitis include redness, warmth, swelling, and pain in the affected area. The affected skin may feel tender and may become increasingly swollen over time. In some cases, individuals may experience fever and chills, indicating a systemic infection.
2. Location: Cellulitis can occur anywhere on the body but is most frequently found on the lower legs and feet. It can also develop on the face, hands, arms, or other parts of the body.
3. Progression: Cellulitis often starts as a small, localized area of redness and swelling but can spread rapidly to involve larger areas of skin. It may appear as a well-defined, red, and inflamed patch that expands outward.
4. Skin Changes: The affected skin may become tight, shiny, and swollen, and it can take on a stretched, glossy appearance. As the condition progresses, the skin may blister, ooze, or develop pustules.
5. Risk Factors: Factors that increase the risk of developing cellulitis include open wounds, breaks in the skin, underlying medical conditions (such as diabetes or weakened immune systems), obesity, and lymphedema (swelling of the limbs due to lymphatic system dysfunction).
6. Diagnosis: Healthcare providers typically diagnose cellulitis based on a clinical examination of the affected area. In some cases, they may order blood tests or a culture of any fluid or tissue that is draining from the infected area to identify the responsible bacteria.
7. Treatment: The primary treatment for cellulitis is antibiotics, which are usually prescribed for 7 to 14 days. It's essential to take the full course of antibiotics, even if the symptoms improve, to ensure complete eradication of the infection. For more severe cases, hospitalization may be required for intravenous (IV) antibiotics and monitoring.
8. Prevention: Preventive measures include practicing good hygiene, promptly cleaning and covering cuts, and avoiding scratching or disrupting insect bites. For individuals at risk of recurrent cellulitis, long-term preventive antibiotics or lymphedema management may be recommended.

Cellulitis can range from mild to severe, and in severe cases, it can lead to complications such as abscess formation, necrotizing fasciitis (a rapidly spreading tissue infection), or the spread of bacteria into the bloodstream (bacteremia or sepsis). Timely treatment with antibiotics is crucial to prevent these complications. Individuals who suspect they have cellulitis, especially if it is rapidly spreading or accompanied by a fever, should seek medical attention promptly.
Dermatitis is a common term used to describe inflammation of the skin. It encompasses a wide range of skin conditions that result in redness, swelling, itching, and other symptoms. Dermatitis can occur in response to various factors, including allergens, irritants, infections, or autoimmune reactions. There are several types of dermatitis, each with its own distinct characteristics:
1. Contact Dermatitis: This type of dermatitis is characterized by an inflammatory reaction that occurs when the skin comes into contact with an irritating substance. It can be further categorized into two subtypes:
- Allergic Contact Dermatitis: This occurs when the skin has an allergic response to a specific substance, such as poison ivy, latex, or certain fragrances. Symptoms often include itching, redness, and the development of small blisters.
- Irritant Contact Dermatitis: This results from exposure to substances that directly irritate the skin, such as harsh soaps, detergents, or chemicals. It can cause redness, itching, and sometimes blistering.
2. Atopic Dermatitis (Eczema): Atopic dermatitis is a chronic and often hereditary condition characterized by dry, itchy, and inflamed skin. It typically appears in childhood and can persist into adulthood. Eczema tends to occur in areas with folds, such as the inside of elbows and behind the knees.
3. Seborrheic Dermatitis: This type of dermatitis affects areas of the body with a high concentration of sebaceous (oil) glands, such as the scalp, face, and upper chest. It often presents as red, scaly, and greasy patches. Seborrheic dermatitis can be associated with dandruff on the scalp.
4. Nummular Dermatitis (Discoid Eczema): Nummular dermatitis is characterized by the presence of round or coin-shaped patches of irritated skin. It is often intensely itchy and can occur anywhere on the body.
5. Stasis Dermatitis: This type of dermatitis occurs in the lower legs and ankles, typically as a result of poor blood circulation. Symptoms may include redness, swelling, and the development of open sores or ulcers.
6. Dyshidrotic Dermatitis: Dyshidrotic dermatitis presents as small, itchy blisters on the hands and feet. The blisters can be painful and may lead to peeling or cracking of the skin.
7. Autoimmune Dermatitis: Some forms of dermatitis, such as lupus or dermatomyositis, result from an autoimmune response where the body's immune system attacks its own skin.
8. Other Forms: There are many other types of dermatitis, including photocontact dermatitis (caused by exposure to sunlight and certain substances), perioral dermatitis (inflammation around the mouth), and more.
Treatment for dermatitis varies depending on the specific type and its underlying causes. Common approaches include the use of topical corticosteroids, moisturizers, antihistamines for itching, and avoiding triggers or irritants. For chronic or severe cases, you may be referred to a dermatologist who may recommend additional treatments or diagnostic tests to identify the cause of the dermatitis.
Radiation Wounds:
Radiation necrosis is a term used in the field of oncology and radiology to describe a condition where healthy tissue in the body, typically adjacent to an area that has been treated with radiation therapy, begins to die or deteriorate as a result of exposure to ionizing radiation. This condition is most commonly associated with the treatment of cancer, where radiation therapy is used to target and kill cancerous cells. While radiation therapy is effective in treating cancer, it can also damage nearby healthy tissues due to the unintended exposure to radiation. The extent and severity of radiation necrosis can vary, and it may take some time to develop after radiation treatment.
Key characteristics of radiation necrosis include:
1. Symptoms: Patients with radiation necrosis may experience a range of symptoms, which can include headaches, cognitive changes, seizures, weakness, or changes in sensation, depending on the location of the affected tissue.
2. Imaging: Diagnosis of radiation necrosis often involves medical imaging, such as MRI or CT scans, which can reveal characteristic patterns of damage and inflammation in the affected area.
3. Treatment: The management of radiation necrosis may involve various approaches, including corticosteroids to reduce inflammation and alleviate symptoms. In more severe cases, additional treatments like hyperbaric oxygen therapy or surgical intervention may be considered.
4. Prevention: Modern radiation therapy techniques aim to minimize radiation exposure to healthy tissues and limit the risk of radiation necrosis. Advanced technology and treatment planning can help reduce the chances of this condition occurring.
Radiation necrosis is a potential side effect of radiation therapy, and its development can vary depending on factors such as the type of cancer, the radiation dose, and the location of the tumor. Patients undergoing radiation therapy are closely monitored, and any symptoms suggestive of radiation necrosis should be reported to their healthcare providers for evaluation and appropriate management.

